Free video consultation | Tuesday 24th February
The next session will be on
Tuesday 24th February 2026
With Dr. Martin Wiese
Book a free video consultation with one of our surgeons, to discuss your symptoms, explore treatment options, and receive expert advice, all from the comfort of your home.
CLINICAL RESEARCH
Scientific foundations of non-mesh hernia surgery
Our approach to hernia surgery is rooted in evidence-based practices and extensive clinical research. This page highlights the scientific studies and expert findings that validate the safety, effectiveness, and long-term benefits of the mesh-free hernia repairs that we offer.
What the research says about non-mesh hernia surgery
Each section on this page focuses on a specific study, providing a summary of its details, the most important takeaways, and how the findings support mesh-free hernia surgery. Every section concludes with why the study matters and how it reinforces our commitment to safe and effective patient care.
1. A landmark study supporting the effectiveness of non-mesh hernia surgery

STUDY DETAILS
A randomised controlled trial involving
1.183 men with primary unilateral
inguinal hernias, comparing the 5-year
outcomes of Shouldice (non-mesh) and
TAPP (mesh) repairs across seven hospitals
in Sweden.
Conducted from 1993 to 1996, this landmark randomised controlled trial (RCT) compared two inguinal hernia repair methods: the traditional, non-mesh Shouldice repair and the then novel, mesh-based TAPP technique. Designed to provide reliable evidence, RCTs ensure accuracy by randomly assigning patients to different treatments. Involving over 1,000 men across seven Swedish hospitals, this trial found similar 5-year recurrence rates—6.6% for TAPP and 6.7% for Shouldice—showing that the Shouldice repair can match the durability of mesh approaches. Recognised as the “gold standard” at the time, Shouldice set the benchmark for comparing newer techniques and this study strongly supports the effectiveness of skilled, non-mesh repairs for long-term success
Key information from this study comparing Shouldice vs. TAPP
- Comparable long-term success:
The Shouldice and TAPP laparoscopic techniques yielded nearly identical recurrence rates after five years, affirming the Shouldice method’s effectiveness in the long-term.
- Dependence on surgical skill:
The study highlighted the importance of surgeon expertise, especially in non-mesh repairs like Shouldice, where precision can greatly impact outcomes. Surgeons with higher performance scores saw significantly lower recurrence rates.
- Natural repair with less risk:
Patients undergoing Shouldice repair experienced outcomes comparable to mesh repairs without the complications sometimes associated with mesh implants.
- Comparable safety and effectiveness across patient types:
The study found that patient factors such as age, occupation, and hernia size did not significantly impact recurrence rates, suggesting that the Shouldice method is broadly effective for various patient profiles. This consistency reinforces that non-mesh repairs can be reliably effective across a wide range of patients, similar to mesh-based methods.
Why this matters
This study provides valuable, long-term data on the effectiveness of non-mesh hernia repair techniques, specifically the Shouldice method, which was once considered the gold standard in hernia treatment. For patients today, it demonstrates that non-mesh repairs can achieve results comparable to mesh-based options in preventing recurrence, offering a natural solution without synthetic mesh. Although Shouldice repair has become less common, its proven durability in studies like this underlines the value of non-mesh approaches for those who prefer to avoid mesh.
Arvidsson D, Berndsen FH, Larsson LG, Leijonmarck CE, Rimbäck G, Rudberg C, Smedberg S, Spangen L, Montgomery A. Randomized clinical trial comparing 5-year recurrence rate after laparoscopic versus Shouldice repair of primary inguinal hernia. Br J Surg. 2005 Sep;92(9):1085-91.↗
2. High risk of chronic pain after mesh repair

STUDY DETAILS
A systematic review of 16 studies
involving 3.086 Lichtenstein mesh repairs.
Chronic pain is a risk associated with all types of surgery, but it’s particularly common in hernia surgery involving mesh. A systematic review of 16 studies involving over 3,000 Lichtenstein open mesh hernia operations, revealed a strong link between chronic postoperative pain and the surgeon’s experience. While experienced surgeons had lower rates of chronic pain compared to their less experienced counterparts, the incidence of chronic inguinal pain remained significant, ranging from 6.9% to 11.7% even among seasoned professionals.
Risk of chronic pain - BioHernia
<
Risk of chronic pain - Experienced mesh surgeons
to
Risk of chronic pain - Inexperienced mesh surgeons
to
Risk of chronic pain after inguinal hernia surgery
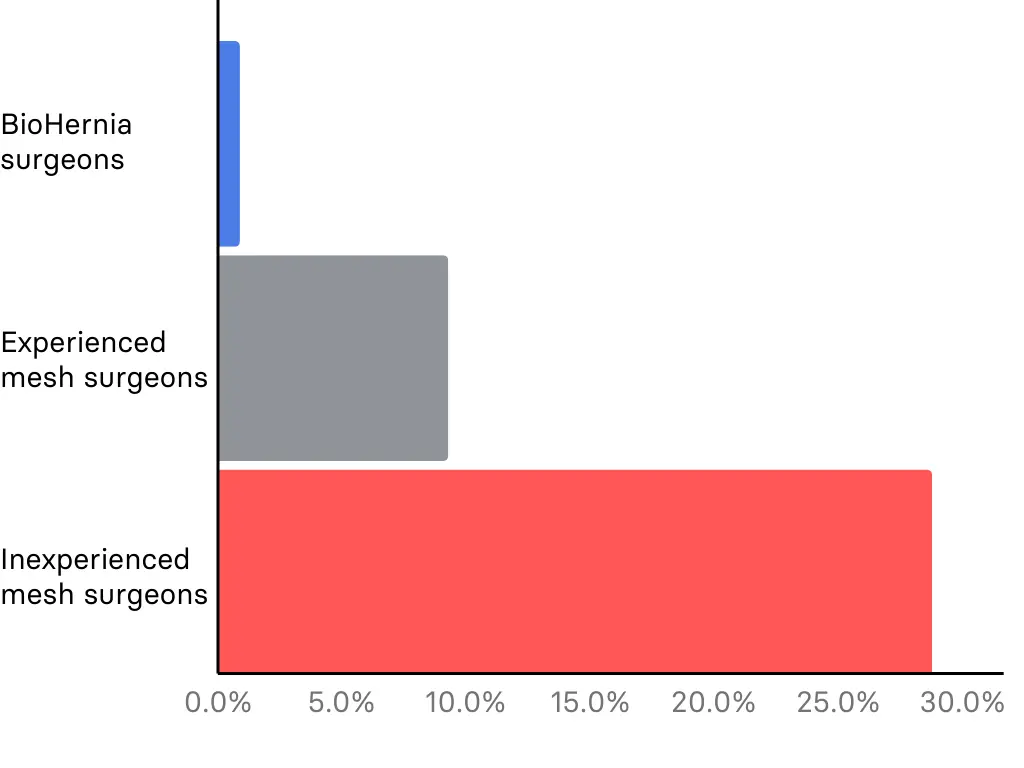
Why this matters
Knowing that even experienced surgeons using the Lichtenstein open mesh technique can have significant rates of chronic pain, our focus on non-mesh, tissue-based repairs offers an alternative that minimises these risks for potential patients.
Lange JF, Meyer VM, Voropai DA, Keus E, Wijsmuller AR, Ploeg RJ, Pierie JP. The role of surgical expertise with regard to chronic postoperative inguinal pain (CPIP) after Lichtenstein correction of inguinal hernia: a systematic review. Hernia. 2016 Jun;20(3):349-56.↗
3. Lower recurrence rates for experienced surgeons.

STUDY DETAILS
A total of 235.192 Ontario residents
who underwent primary elective inguinal hernia
surgery in an Ontario hospital between 1993 and 2007
were studied using population-based
administrative health data. The study compared
patients treated at a large hernia specialty
hospital, Shouldice Hospital, with those treated
at general hospitals to determine the risk
of recurrence.
A study found that inguinal hernia repairs performed at the Shouldice Hospital in Toronto (specialised in mesh-free hernia repairs) had a significantly lower risk of recurrence, compared to repairs done at general hospitals (usually done with mesh).
Comparison of success rates
Success rate for specialised mesh-free hernia centers like BioHernia & Shouldice
Success rate of general hospitals using mesh
Recurrence risk after inguinal hernia surgery

Why this matters
The main argument of the pharmaceutical industry for using meshes in inguinal hernia repairs is the high recurrence risk. This study demonstrates that specialised centers, such as the Shouldice Hospital or BioHernia, achieve lower recurrence rates even without using mesh. This challenges the necessity of mesh implants and supports the effectiveness of mesh-free repairs when performed by experienced specialists, offering patients safer alternatives with fewer complications.
Malik A, Bell CM, Stukel TA, Urbach DR. Recurrence of inguinal hernias repaired in a large hernia surgical specialty hospital and general hospitals in Ontario, Canada. Can J Surg. 2016 Feb;59(1):19-25. ↗
4. Lower inflammatory response after mesh-free hernia repair
This study highlights that the mesh-free Shouldice repair technique is the least traumatic procedure in terms of immune response and inflammation, specifically compared to endoscopic hernia repairs.
The graphs below illustrate the differences in inflammatory response between the Shouldice and endoscopic TEP methods across four key parameters.
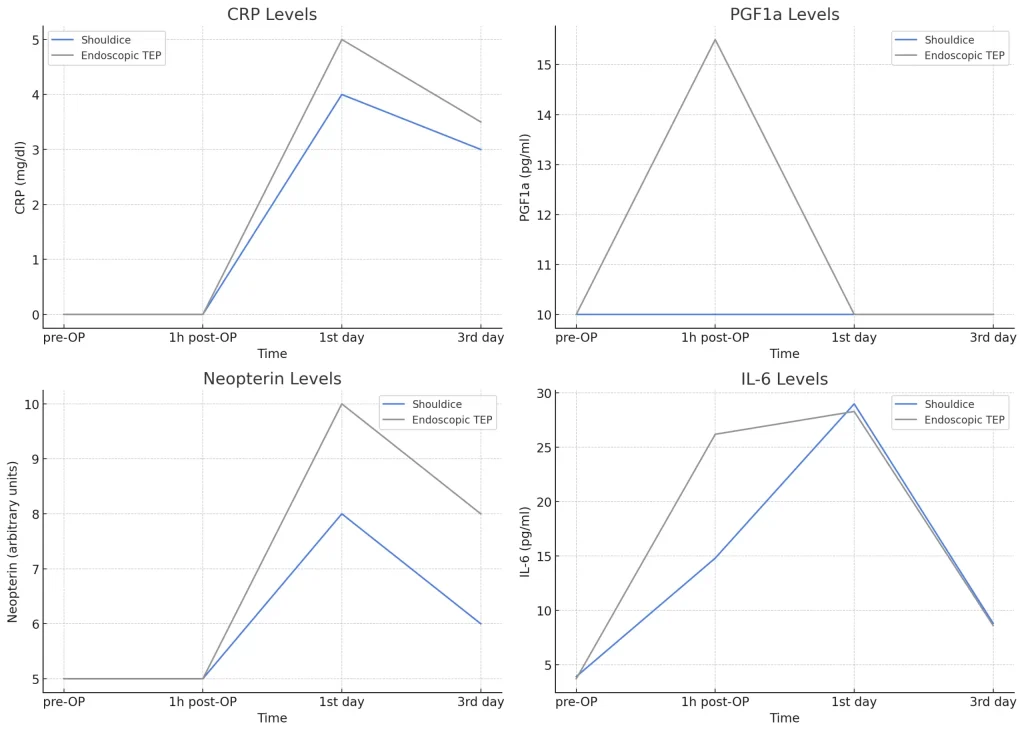
Why this matters
This finding underscores the benefits of our mesh-free hernia repair approach, emphasising its minimal impact on the body and its effectiveness in promoting a smoother, less inflammatory recovery process.
Schwab R, Eissele S, Brückner UB, Gebhard F, Becker HP. Systemic inflammatory response after endoscopic (TEP) vs Shouldice groin hernia repair. Hernia. 2004 Aug;8(3):226-32. ↗
5. Higher risks for women
The study, which was co-authored by our own surgeon Dr. Andreas Koch, explores the prevalence, risk factors, and management strategies of groin hernias in women. Groin hernias are less common in women than men, with a lifetime risk of 3-5.8% for women compared to 27-42% for men. However, women are also more likely to experience chronic postoperative pain, making careful surgical planning and follow-up essential.
Key information from the study on hernia surgery risks for women
Higher Incidence of Femoral Hernias:
Women have a significantly higher proportion of femoral hernias compared to men, ranging from 16.7% to 37%. Femoral hernias are more prone to complications and often require emergency surgery, which has higher associated risks.
Emergency Surgery Rates:
The rate of emergency procedures in women with groin hernias is 14.5% to 17%, which is 3 to 4 times higher than in men. This high rate underscores the need for timely elective repairs to avoid emergency situations.
Higher Mortality Risk:
The mortality rate following emergency femoral hernia repair is 7 to 10 times higher for women compared to elective procedures. This is due to the higher risk of complications and the generally poorer health status of patients requiring emergency surgery.
Chronic Postoperative Pain:
Studies have shown that 24.2% of women report experiencing chronic postoperative pain following femoral hernia mesh repair. This is significantly higher compared to men, who report an incidence rate of around 5.5%.
Recurrence Rates:
Women have higher recurrence rates of hernias post-surgery, often due to femoral hernias being overlooked during the primary operation. Ensuring thorough diagnosis and appropriate treatment during the initial surgery is crucial to reduce recurrence.
Impact on Quality of Life:
The combination of higher rates of chronic pain and recurrence can severely affect women’s quality of life post-surgery. Proper surgical techniques and careful postoperative care are essential to mitigate these risks.
Why this matters
Understanding the risks women face in hernia surgery, as highlighted by this study, is crucial for improving patient outcomes. Women have higher rates of femoral hernias and emergency surgeries, leading to increased morbidity and mortality. Chronic postoperative pain and higher recurrence rates significantly impact their quality of life. These insights emphasise the need for tailored surgical approaches and careful postoperative care to reduce these risks and enhance recovery for women.
Köckerling F, Koch A, Lorenz R. Groin Hernias in Women-A Review of the Literature. Front Surg. 2019 Feb 11;6:4. ↗
6. Nerves entrapped by hernia mesh
Another study, co-authored by our surgeon Dr. Andreas Koch, revealed that patients with mesh repairs experiencing chronic pain had three times more nerve growth into the mesh compared to those without pain. This chronic pain is often due to nerve branches growing into and becoming trapped within the mesh, leading to significant discomfort.
Microscopic images show various nerve branches growing into the mesh.
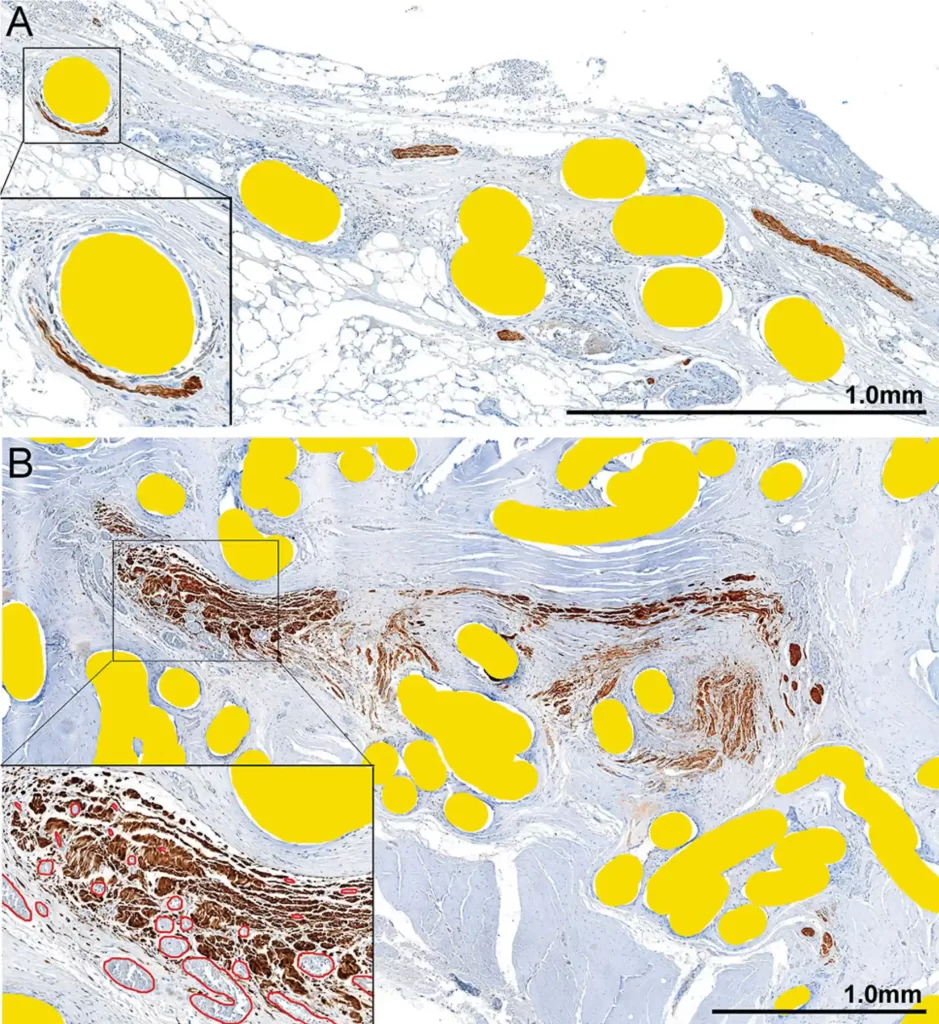
A brown stain highlights the cells of the peripheral nerves, while mesh fibers are shown in yellow for clarity.
- Image A: Smaller nerve branches grow through the mesh pores, with one branch distorted by a mesh filament (see the enlarged insert).
- Image B: A larger nerve is seen within the mesh folds of a plug. The right half of the image shows the nerve splitting into smaller sections and being distorted into a traumatic neuroma. The insert highlights a part of the nerve near the neuroma, showing enlarged, congested blood vessels outlined in red. The nerve is affected both externally by the mesh filaments and internally by the swollen vessels.
Why this matters
These findings underscore the importance of carefully considering mesh design and surgical techniques to prevent nerve-related chronic pain.
Bendavid R, Lou W, Grischkan D, Koch A, Petersen K, Morrison J, Iakovlev V. A mechanism of mesh-related post-herniorrhaphy neuralgia. Hernia. 2016 Jun;20(3):357-65. ↗
7. Higher risks of chronic pain after mesh repair
This study found that chronic pain after groin hernia surgery was more common in patients who had mesh repairs compared to those who had non-mesh repairs. Specifically, 13.9% of patients with mesh repairs experienced chronic pain (236 out of 1693 patients), while only 4.4% of those with non-mesh repairs did (3 out of 68 patients). However, because there were very few patients in the non-mesh group, the researchers could not definitively say that the difference was statistically significant.
The study also does not detail the specific non-mesh techniques used, which is a limitation in interpreting the findings. Additionally, the study does not account for the skill level of the surgeons, which is especially important for non-mesh repairs as few surgeons are highly experienced in these techniques.
The graphs below illustrate the differences in chronic pain between mesh-free repairs and mesh repairs.
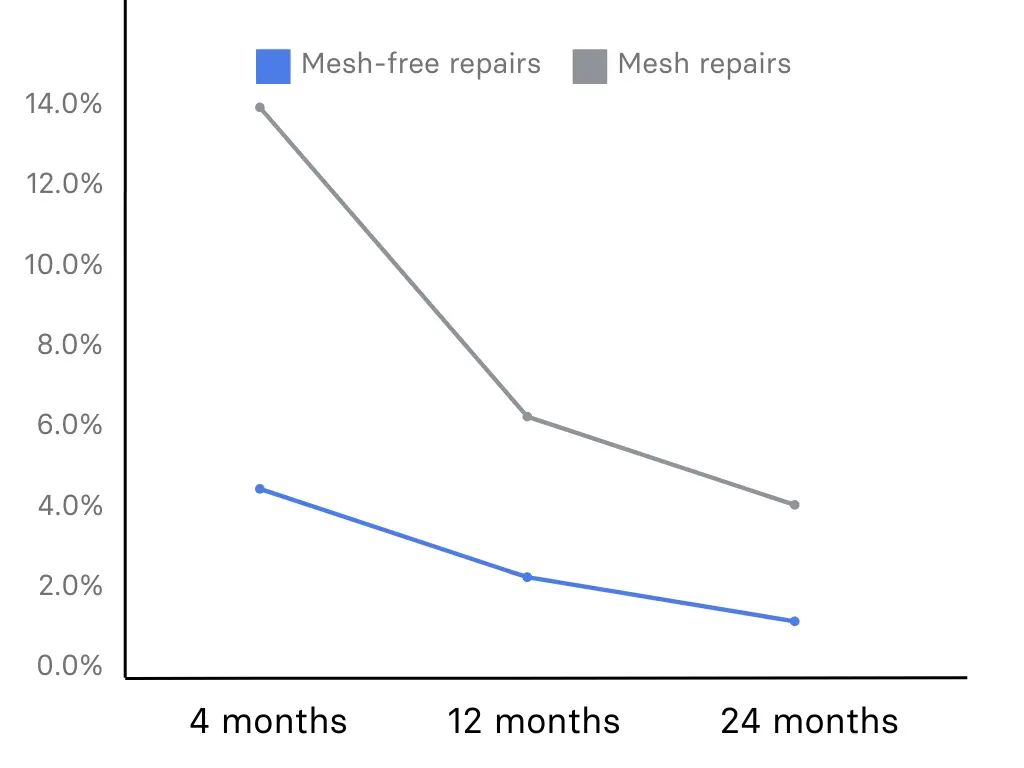
Why this matters
Understanding the difference in chronic pain between mesh and non-mesh hernia repairs is crucial because it directly impacts the choice you make as a patient. Chronic pain can severely affect daily activities and mental health, making it essential to choose the best surgical method.
Bande D, Moltó L, Pereira JA, Montes A. Chronic pain after groin hernia repair: pain characteristics and impact on quality of life. BMC Surg. 2020 Jul 6;20(1):147. ↗
Advancing the future of hernia surgery
Our surgeons are deeply passionate about advancing hernia care and consistently remain at the forefront of innovation. Through scientific research and active contributions to the global community of hernia surgeons, they are shaping the future of hernia care and restoring mesh-free surgery to its rightful place in the field. Their commitment to innovation, scientific integrity, and independence from the pharmaceutical industry, ensures that we continue to provide cutting-edge, evidence-based solutions without the use of mesh.
Frequently asked questions
How does the research conducted by BioHernia surgeons benefit patients?
The research conducted by our surgeons directly benefits patients by improving the techniques and outcomes of hernia surgery. Conducting research forces our surgeons to focus on and better understand specific aspects of a technique or human anatomy, which in turn improves their ability to perform operations. By integrating the latest scientific findings into clinical practice, we can offer more effective, safer, and less invasive treatment options. This commitment to research and innovation ensures that you receive the best possible care tailored to your individual needs.
How are BioHernia surgeons involved in scientific research?
Our surgeons are actively engaged in scientific research focused on advancing hernia surgery techniques. They conduct studies, publish findings in reputable medical journals, and collaborate with other experts in the field to develop innovative, effective, and safe hernia repair methods. Importantly, the research conducted by our surgeons is independent and not financed by big pharmaceutical companies, ensuring unbiased and patient-centered advancements.
Do BioHernia surgeons contribute to policy-making in hernia surgery?
Yes, our surgeons play a significant role in shaping policies related to hernia surgery. They attend, speak at, and contribute to national and international hernia congresses, and participate in the development of clinical guidelines. Our surgeons are among the few who still advocate for mesh-free repairs in these guidelines, ensuring that mesh-free repairs remain recognised and do not become obsolete in the field of hernia surgery.
8. Further reading
For those interested in delving deeper into the field of hernia surgery, we have compiled a selection of scientific articles and papers. These resources provide additional insights and detailed information about the latest advancements and research in hernia treatment. Click on the links below to explore further.
1.
Nienhuijs SW et al (2008) An overview of the features influencing pain after inguinal hernia repair. Int J Surg (London, England)
3.
Bischoff JM et al (2013) Long-term follow-up after mesh removal and selective neurectomy for persistent inguinal postherniorrhaphy pain.
4.
Lorenz R, Arlt G, Conze J, Fortelny R, Gorjanc J, Koch A, Morrison J, Oprea V, Campanelli G. Shouldice standard 2020: review of the current literature and results of an international consensus meeting.
5.
Bay-Nielsen M, Perkins FM, Kehlet H (2001) Pain and functional impairment 1 year after inguinal herniorrhaphy: a nationwide questionnaire study.
6.
Nienhuijs S, Staal E, Strobbe L, Rosman C, Groenewoud H, Bleichrodt R (2007) Chronic pain after mesh repair of inguinal hernia: a systematic review.
7.
Aasvang EK, Kehlet H (2009) The effect of mesh removal and selective neurectomy on persistent postherniotomy pain.
8.
Amid PK, Chen DC (2011) Surgical treatment of chronic groin and testicular pain after laparoscopic and open preperitoneal inguinal hernia repair.
10.
Gukas ID, Massouh F (2011) Serious life threatening complica- tion 5 years after laparoscopic totally extraperitoneal hernia repair: case report and discussion of the literature.
