Free video consultation | Tuesday 24th February
The next session will be on
Tuesday 24th February 2026
With Dr. Martin Wiese
Book a free video consultation with one of our surgeons, to discuss your symptoms, explore treatment options, and receive expert advice, all from the comfort of your home.
The Marcy repair explained
Developed in the 1870’s by Dr. Henry O. Marcy (1837-1924), a Harvard medical school graduate and American Civil War veteran, the Marcy technique has withstood the test of time because of its simplicity and effectiveness. This technique focuses on narrowing the internal ring, specifically in cases of indirect inguinal hernias. When performed by an experienced surgeon, it offers excellent success rates for selected patients. We reserve this method exclusively for women, children, and in rare cases for adolescent men who have small hernias, as it requires strong inguinal floor tissue—typically found only in these patient groups. The illustrations below describe the operation in an adult women.
Considerations for women
Historically, most groin hernia treatments have been male-focused, leading to a gap in specialised care for women. BioHernia is committed to bridging this gap by providing a hernia repair that is meticulously adapted to meet the distinct needs of women. This tailored approach ensures both effective treatment and respectful acknowledgment of women’s specific anatomical and physiological requirements.
1. Assessment of femoral hernias
Femoral hernias are more common in women, with a prevalence of around 15%, they are often overlooked when repairing inguinal hernias. Recognising this, we conduct a thorough assessment to accurately identify and treat a femoral hernia, if present.
2. Protection of the round ligament
The round ligament in women, similar to the spermatic cord in men, is an important structure that runs through the inguinal canal and helps keep the uterus stable. Typically, in an inguinal hernia procedure, this ligament is cut. However, we take extra care to protect this ligament, aiming to avoid any harm to it and maintain the structural integrity of the uterus.
3. Tailored approach for women
Recognising that women’s anatomy in the groin area is distinctively different and their tissues are often more resilient than in men, we tailor our approach accordingly. Our surgeons’ extensive experience allows us to adapt our techniques during the operation. This flexibility allows us to switch to less invasive techniques where possible, ensuring a procedure that’s not only effective but also customised to your unique characteristics.

Starting your repair
Following the administration of either a general or local anaesthetic, we start the inguinal hernia repair by making a small 3 to 5cm incision in the lower abdominal area. Throughout the procedure, a dedicated anaesthetist is on hand to ensure your comfort and well-being. The incision is in the lower abdominal area, ensuring that any resulting scar remains discreet, hidden when swimwear or underwear is worn.

Round ligament
of the uterus
Subcutaneous fat
External oblique aponeurosis
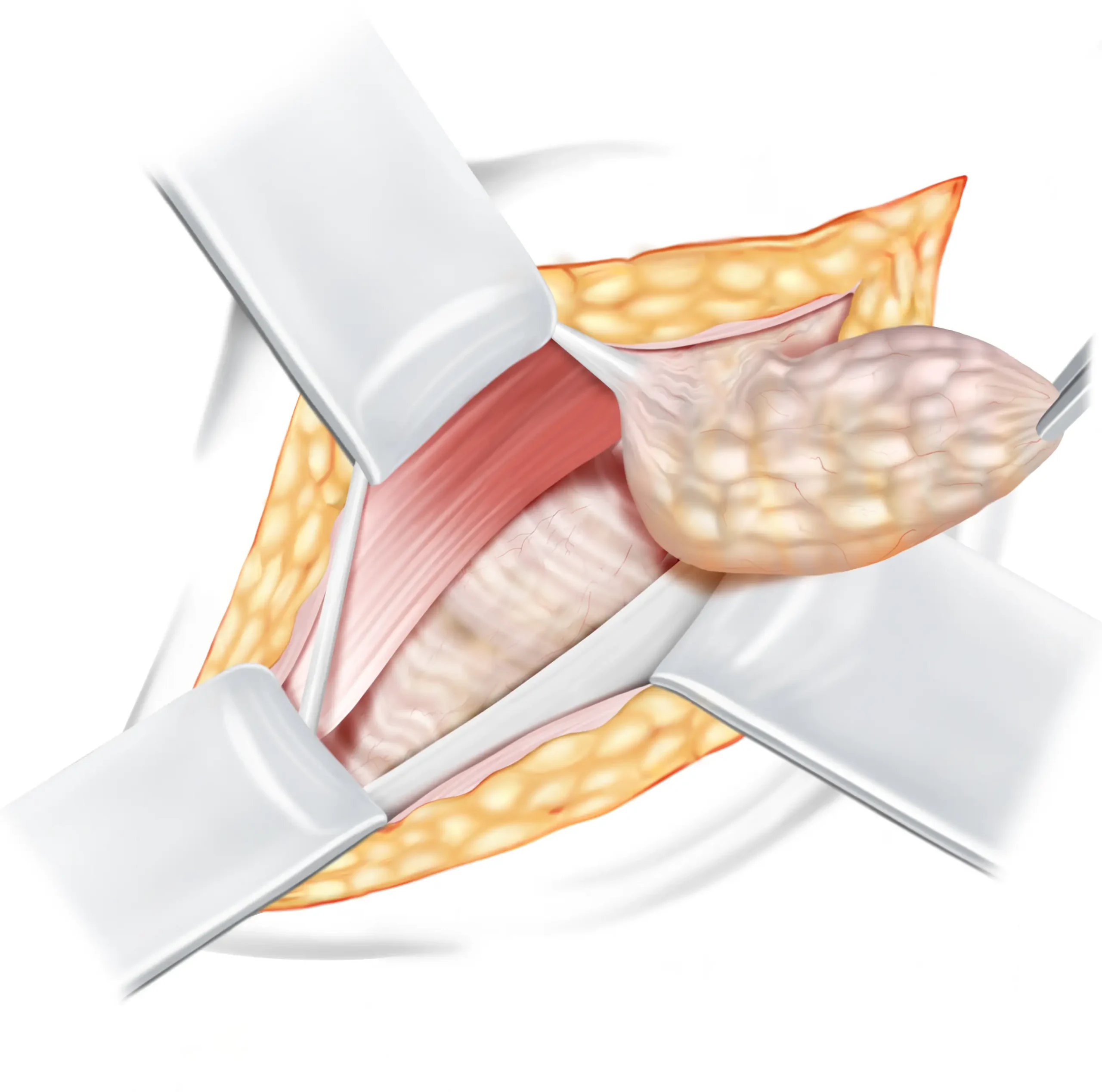
Opening the inguinal canal
The first tissue we encounter is the aponeurosis of the external oblique muscle ↓, which forms the roof of the inguinal canal ↓ . To gain access to the inguinal canal for the repair, we need to open this tissue. It is important to note that opening the external oblique aponeurosis (EOA) does not have any negative impact on its functionality, as it will be closed again during the final step of the operation. Once opened, the round ligament of the Uterus↓ is safely pulled to the side and the two flaps of the external oblique aponeurosis are carefully retracted as they will be utilised later in the repair process.
DETAILED EXPLANATION
The external oblique aponeurosis is incised from the superficial inguinal ring past the deep inguinal ring. After opening, the upper leaf of external oblique is slightly elevated and undermined with a finger, to free it from the underlying internal oblique muscle.
Round ligament
of the Uterus
Subcutaneous fat
Indirect hernia sac
(containing fat or bowel)
Inguinal ligament
Internal oblique muscle
Transversalis fascia
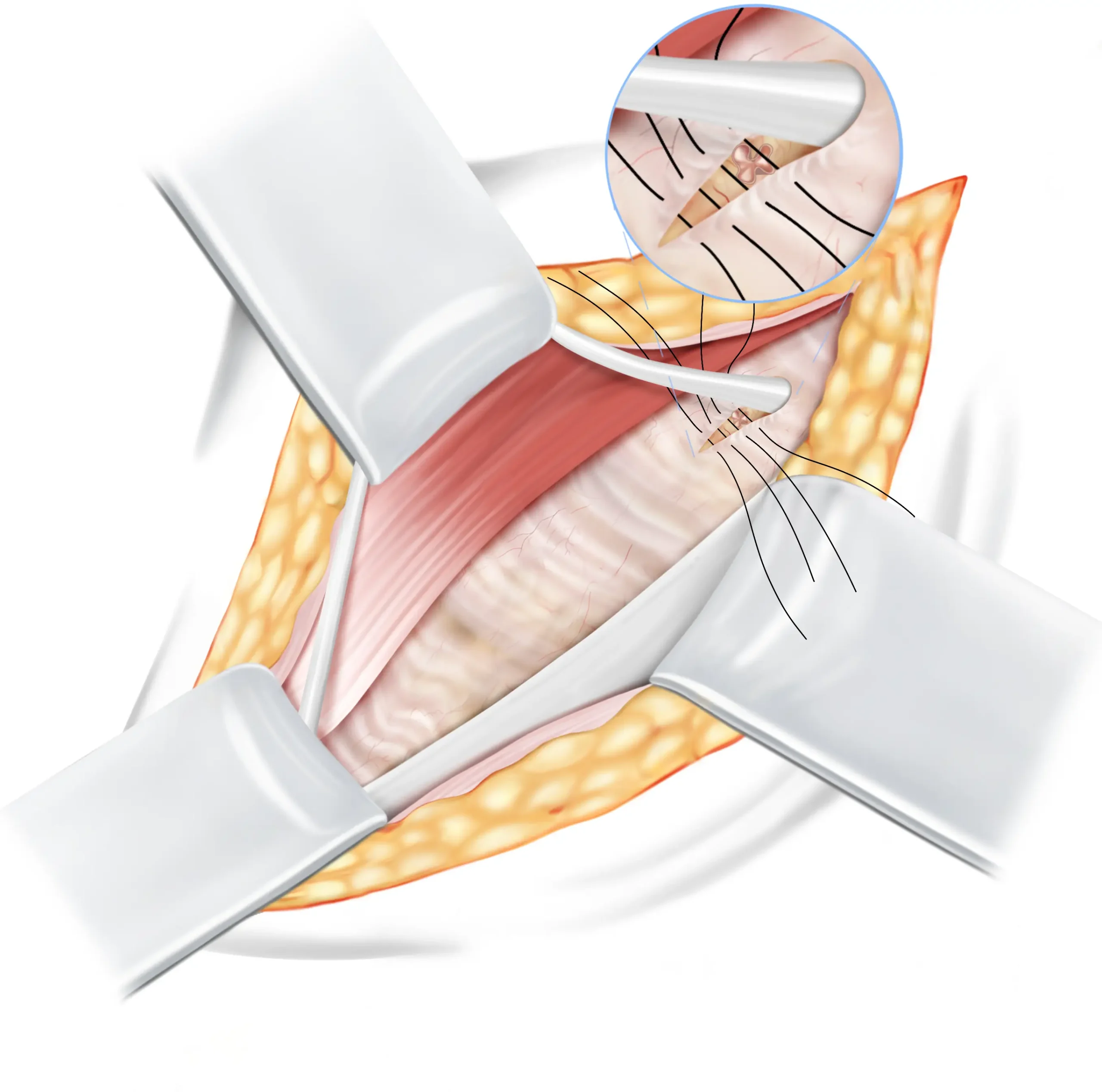
Hernia sac management
The majority of inguinal hernias in women, are indirect. This means that the internal ring ↓ is dilated, and allows a sac of intestines or fatty tissue to protrude, causing a bulge in the groin. The round ligament is pulled to the side, and after the contents of the hernia sac ↓ are inspected, it is reduced back into the abdomen.
DETAILED EXPLANATION
The majority of inguinal hernias in women are indirect. Given the strong nature of the inguinal floor in women, we believe there is no need to open the inguinal floor if there is no indication of a direct inguinal hernia or femoral hernia. In case of a direct hernia, the transversalis fascia is opened and a Shouldice repair is performed (or in some cases the transversalis fascia is not opened and a Desarda repair is done). The hernia sac is opened, and its contents are inspected and reduced to the abdominal cavity. Any non-viable tissue is excised. The hernia sac is then ligated at its base, ensuring there’s no constriction of the associated structures, especially in women, the round ligament. The round ligament remains intact and undamaged.
Round ligament
of the Uterus
Subcutaneous fat
Inguinal ligament
Internal oblique muscle
Transversalis fascia
Dilated internal ring
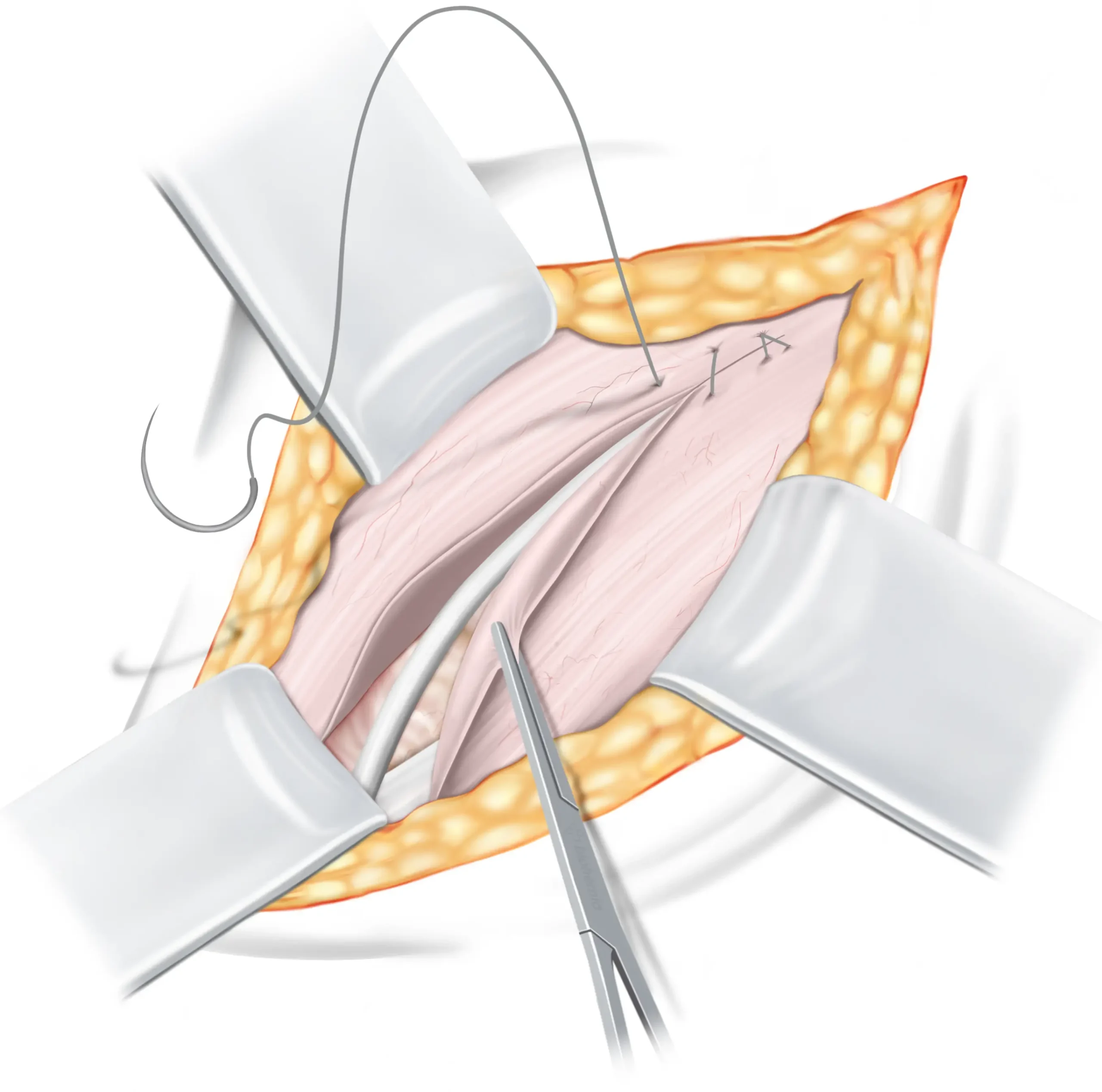
The Marcy repair
Having reduced the hernia sac in the preceding step, we are left with a dilated internal ring that needs tightening to prevent the development of a new hernia. In young, healthy women, the inguinal floor is resilient, which is why we believe that there is no need to open it and construct a layered repair as we would in men. The defect is repaired using the Marcy technique, whereby sutures are used to narrow the internal ring to its normal anatomical size. For clarity, we have magnified the internal ring in this illustration. This method proves to be much less invasive for women and facilitates a speedier recovery compared to our other operation techniques.
DETAILED EXPLANATION
The internal ring is tightened using the Marcy technique with interrupted absorbable sutures. When tightening the internal ring, one must be careful with the genital branch nerves, which runs below. Care is taken to ensure that there is no constriction of the structures passing through the internal ring, avoiding damage to the round ligament in women.
Round ligament
of the Uterus
Subcutaneous fat
External oblique aponeurosis
Finalising the repair
The round ligament is carefully returned to its natural position, and the inguinal canal is closed by bringing together the fascia of the external oblique muscle and securely suturing it with resorbable sutures.
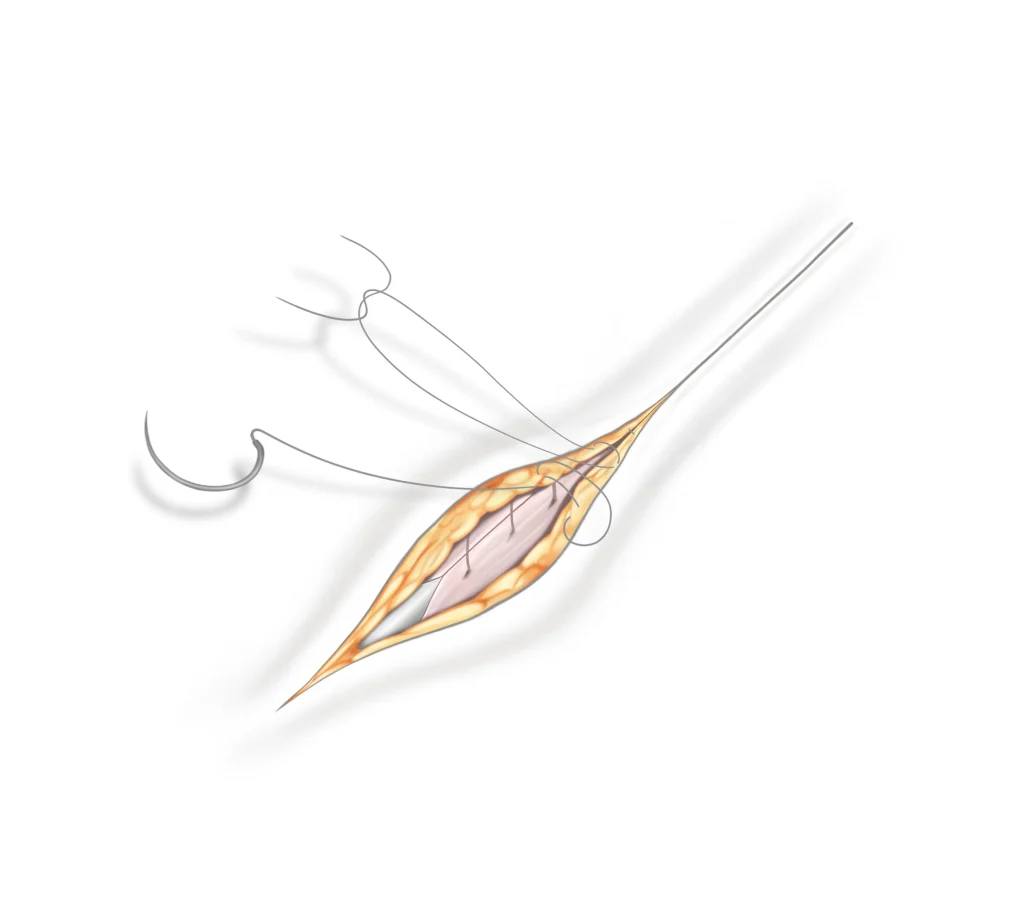
Closing the skin
After the procedure, the incision is closed using sutures that the body naturally absorbs. Therefore, there is no need for you to return for suture removal, as these sutures dissolve on their own. Local anaesthetics will also be applied, which could make the area look somewhat swollen after the operation, but this is a typical response and helps reduce pain after the operation.
Wound care
In the final steps, medical glue and Steri-Strips are applied to your wound. These strips aid in holding the wound’s edges together, minimising potential scarring during the healing process. You can safely remove the strips after one week.
DISCLAIMER
The illustrations displayed on this page have been adjusted in size—some enlarged and others reduced—to enhance understanding. They are intended to provide a simplified explanation of the operation technique and do not accurately portray the complex nature of human anatomy, nor do they convey the intricate challenges encountered during actual surgical procedures. Within the human body, everything is interlinked, making the identification of tissues, nerves, and blood vessels more challenging than what is suggested by the illustrations. Consequently, considerable experience and surgical skill are essential to accurately and effectively perform the operation technique illustrated.
Frequently asked questions
1. What makes the Marcy repair different from other hernia treatments?
The Marcy repair is distinguished by its mesh-free technique, which avoids using synthetic mesh to reinforce the abdominal wall. Instead, it involves suturing the dilated internal ring of the inguinal canal back to its normal size using the patient’s own tissues, thereby reducing the risk of complications such as infection or mesh rejection. This method is considered less invasive compared to other surgical techniques as it involves fewer alterations to the surrounding tissues, leading to a quicker recovery and less postoperative pain.
Specifically effective for indirect inguinal hernias, the Marcy repair targets the hernia sac that protrudes through the internal inguinal ring. It directly addresses and repairs the defect without the need for extensive dissection or reinforcement with foreign materials. When performed correctly in suitable candidates, the Marcy repair has demonstrated lower recurrence rates by effectively restoring the natural anatomy of the inguinal canal, which helps prevent the hernia from recurring.
The Marcy repair is particularly recommended for women and younger patients, as well as those with smaller hernias, due to its reliance on strong, healthy tissue and its tissue-conservative nature. This makes it a safer and less aggressive treatment option, especially suited to patients looking for minimal surgical intervention.
2. What is the difference between a direct and indirect hernia?
A direct hernia occurs due to a weakness in the abdominal wall, commonly seen in older individuals. An indirect hernia, however, protrudes through the inguinal canal following the spermatic cord, and is often a condition present from birth. In terms of prevalence, indirect hernias are more common than direct hernias, especially in women. The Marcy repair is specifically designed to fix small indirect inguinal hernias only. If a direct hernia is found during your operation, our surgeons can switch to a different type of repair like the Shouldice or Desarda repair.
3. Is the Marcy repair suitable for all types of hernias?
The Marcy repair is not suitable for all types of hernias. It is specifically designed for treating small, indirect inguinal hernias. These are hernias where the hernial sac protrudes through a naturally occurring weak spot in the internal inguinal ring. The Marcy repair effectively narrows this opening back to its normal size using sutures, which restores the integrity of the inguinal canal. For this we need strong connective tissue, which is typically only found in women and young adults.
However, for other types of hernias, such as direct inguinal hernias, femoral hernias, or larger or more complex hernias, different surgical approaches are required. These other types need other techniques that provide stronger reinforcement to the weakened area. Each type of hernia has unique characteristics and requires a tailored approach based on your specific anatomy and needs. Therefore, it’s crucial to have a thorough evaluation by one of our specialists to determine the most appropriate treatment option.
4. Are any nerves cut during the operation?
In the inguinal area, there are three nerves: the ilioinguinal nerve, the genital branch of the genitofemoral nerve, and the iliohypogastric nerve. During our inguinal hernia operations, none of these nerves are cut. We take the utmost care to preserve these nerves, ensuring the best possible outcomes for our patients. This careful approach minimises the risk of nerve-related complications and contributes to a smoother recovery.
5. What happens when a femoral hernia is found during the operation?
If a small femoral hernia is discovered during your operation, we can often address it without the need for mesh, especially if it is small. For larger hernias, we may need to use a Phasix mesh, which is absorbable. This type of mesh gradually dissolves and is safely absorbed by your body over time. It’s made from the same material as resorbable sutures, which naturally breaks down through a process known as hydrolysis.
We strive to identify any potential femoral hernias during your pre-operative examination.
6. How long is the recovery period after a Marcy repair?
The recovery period after a Marcy repair is generally shorter compared to more invasive hernia surgery techniques. Typically, patients can expect to return to light daily activities within a few days to a week after the procedure. However, the total recovery time can vary depending on several factors such as the patient’s overall health, the exact nature of the hernia, and how strictly they follow post-operative care instructions.
Most patients can resume normal activities, including going back to work, within 1 week if their job is not physically demanding. For those involved in heavier physical activities or jobs that require strenuous labor, a longer recovery period of 4 weeks may be necessary to ensure complete healing and to avoid complications.
Individual recovery may vary, and it’s important to follow the specific guidance provided by your surgeon.
7. What are the success rates and potential risks associated with the Marcy repair?
The Marcy repair is known for its high success rates, especially when performed on suitable candidates with small, indirect inguinal hernias. Success rates can vary, but generally, this procedure is highly effective with a success rate often exceeding 98%. The technique’s effectiveness in restoring the natural anatomy of the inguinal canal significantly reduces the likelihood of hernia recurrence. However, as with any surgical procedure, there are potential risks, such as infection, bleeding, and post-operative pain. The risk of chronic pain or discomfort is generally significantly lower compared to mesh repairs. It’s important for you to discuss individual risks and concerns with our team to gain a comprehensive understanding of the procedure.
8. Does the Marcy repair also work for recurrent hernias?
The Marcy repair can be an option for recurrent hernias, particularly if the initial hernia was small and the recurrence is also a small, indirect inguinal hernia.
However, the suitability of the Marcy repair for a recurrent hernia depends on various factors, including the specific characteristics of the hernia, the patient’s overall health, and most of all the technique used for previous surgeries. In cases where the tissue has been weakened or there are larger defects, alternative methods could be more appropriate.
If you have a recurrent inguinal hernia, it’s important for you to consult with our specialists who can assess the specific circumstances and recommend the most effective treatment approach tailored to your needs.
9. Does the Marcy repair cause tension in the groin?
The idea of a “tension-free” repair is more of a marketing term used by various hernia repair methods to highlight their approach. However, a certain degree of tension is inherent in the nature of hernia repairs. This includes the Marcy repair, as well as other natural-tissue and mesh-based techniques.
The Marcy repair is designed to introduce minimal tension, especially when compared to other hernia repair methods. In this procedure, the dilated internal ring of the inguinal canal is sutured back to a normal size using the patient’s own tissues, without the need for external mesh or extensive tightening that could lead to increased tension.
Since the Marcy repair primarily involves suturing in connective tissue to restore the internal ring to its appropriate size and not pulling or stretching tissues excessively, it typically results in minimal postoperative tension in the groin area.
Terminology
Learn more about the hernia terms used on this page, in our simple, easy-to-understand glossary.
External oblique aponeurosis
The external oblique aponeurosis functions as a connecting tissue that links the external oblique muscle to the bones in the abdominal region (the lower ribs and the pelvis). Think of it as a robust sheet that fastens the muscle to its surroundings. This connection offers stability and support to the muscle, enhancing the overall strength and functionality of your abdominal area. While its main role is in muscle attachment, it also contributes to the structural integrity of the abdominal wall.
The inguinal canal
The inguinal canal is a canal located in the lower abdomen, next to the groin. It acts as a pathway for structures like blood vessels and the spermatic cord to pass through. This canal plays an important role in male anatomy and sexual functionality.
The internal ring
Consider the internal ring to be a sort of gateway in the lower abdomen, near the groin. It’s a natural opening in the abdominal wall. This opening allows blood vessels and the spermatic cord to travel between your inner abdomen and the groin area. The internal ring, similar to how a door allows you to go between rooms, allows various parts of the body to move around where they need to be. It’s a natural component of how our bodies are constructed.
Hernia sac
A hernia sac is a delicate, pouch-like structure that develops when a section of an organ or fatty tissue pushes through a vulnerable area or gap in the surrounding muscle or connecting tissue. Think of it as a small pocket that accommodates the bulging tissue. The size and location of hernia sacs can differ depending on the type of hernia.
The inguinal ligament
Imagine the inguinal ligament as a kind of strong, flexible band that runs from the front of your hip bone to the pubic bone. It’s like a support belt for your lower abdomen and groin area. This ligament helps hold things in place and provides stability to the region. Just like how a belt supports your trousers, the inguinal ligament supports the structures in your lower belly, making sure everything stays where it should be.
Internal oblique muscle
The internal oblique is one of the three layers of muscles that make up your abdominal wall. In the inguinal area, the internal oblique muscle is sandwiched between the external oblique muscle and the transverse abdominis muscle. Think of the internal oblique muscle as a layer of muscle in your abdomen, just beneath your skin and the surface muscles. It’s like a hidden layer that adds strength and support to your belly. This muscle helps you twist, bend, and move your torso.
The round ligament of the Uterus
The round ligament is a strong connective tissue that supports and stabilises the uterus and stretches from each side of your uterus to the groin area. You can think of it almost like the drawstrings of a hoodie, helping to maintain the position of the uterus by connecting it to the front of your pelvic area. Just as drawstrings help keep a hoodie snug and properly fitted, the round ligaments help keep the uterus aligned and stable as it grows during pregnancy, ensuring comfort and support as your body changes.
Resorbable sutures
Resorbable sutures are designed to have a controlled rate of breakdown in your body. This means that over time, the sutures gradually dissolve and get absorbed by your body. They’re made from a substance that breaks down through a natural process called hydrolysis.
Further reading
Explore our curated selection of scientific literature for a deeper understanding of the Marcy repair.
- Biographical sketch of Dr. Henry O. Marcy (1896). Concord, N.H.
- Marcy, H.O. (1879) The radical cure of hernia by the antiseptic use of the carbolized catgut ligature. Cambridge Mass.: Printed at the Riverside Press.
- Köckerling F, Koch A, Lorenz R. Groin Hernias in Women-A Review of the Literature. Front Surg. 2019 Feb 11;6:4. ↗
- Thairu NM, Heather BP, Earnshaw JJ. Open inguinal hernia repair in women: is mesh necessary? Hernia. 2008 Apr;12(2):173-5; discussion 217. ↗
- Schumpelick V. Does every hernia demand a mesh repair? A critical review. Hernia. 2001 Mar;5(1):5-8. ↗
- Bendavid R. New techniques in hernia repair. World J Surg. 1989 Sep-Oct;13(5):522-31. ↗
- Koch A, Lorenz R, Meyer F, Weyhe D. Hernia repair at the groin—who undergoes which surgical intervention? Zentralbl Chir. 2013;138:410–7. ↗
- Köckerling F, Lorenz R, Hukauf M, Grau H, Jacob D, Fortelny R, Koch A. Influencing Factors on the Outcome in Female Groin Hernia Repair: A Registry-based Multivariable Analysis of 15,601 Patients. Ann Surg. 2019 Jul;270(1):1-9. ↗
- Bendavid R, Howarth D. Transversalis fascia rediscovered. Surg Clin North Am. 2000 Feb;80(1):25-33. ↗
- Pivo S, Huynh D, Oh C, Towfigh S. Sex-based differences in inguinal hernia factors. Surg Endosc. 2023 Nov;37(11):8841-8845. ↗
- Marcy, H.O. (1897) The cure of inguinal hernia in the male: Read at the forty-second annual meeting of the Ohio State Medical Society, at Cleveland, Ohio, May 19, 1897. Norwalk, OH: Laning Printing Company.
